Spinal fusion
| Spinal fusion | |
|---|---|
| Intervention | |
 A 24-year-old male showing a normal kyphosis curve after a 13-level spinal fusion to correct Scheuermann's disease | |
| ICD-9-CM | 81.0 |
| MeSH | D013123 |
| MedlinePlus | 002968 |
Spinal fusion, also called spondylodesis or spondylosyndesis, is a neurosurgical or orthopedic surgical technique that joins two or more vertebrae. Surgeons use supplementary bone tissue—either from the patient (autograft) or a donor (allograft)—or artificial bone substitutes in conjunction with the body's natural bone growth (osteoblastic) processes to fuse two or more adjoining vertebrae.
Spinal fusion treats a variety of pathological conditions to eliminate abnormal motion of the vertebrae that causes pain, neurological deficit, or spinal deformity. Common conditions incorporating spinal fusion in their surgical treatment are spinal stenosis, spondylolisthesis, cervical discopathy, spinal fractures, scoliosis, and kyphosis.
Medical uses
Spinal fusion is done most commonly in the lumbar region of the spine, but it is also used to treat cervical and thoracic problems. The indications for lumbar spinal fusion are controversial.[1] People rarely have problems with the thoracic spine because there is little normal motion in the thoracic spine. Spinal fusion in the thoracic region is most often associated with spinal deformities, such as scoliosis and kyphosis.
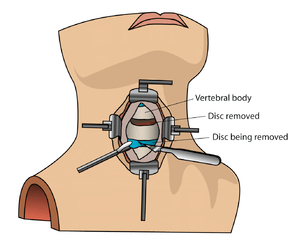
Cervical spinal fusion can be performed for several reasons. Following injury, this surgery can help stabilize the neck and prevent damage to the spinal cord. Additionally, cervical spinal fusion can be used to remove or reduce pressure on nerve roots caused by bone ingrowth osteophytes or herniated intervertebral disks.
Patients who require spinal fusion have either neurological deficits or severe pain that hasn't responded to conservative treatment. Spinal fusion surgeries are also common in patients who suffer from moderate to severe back deformities that require reconstructive surgery.
When performing spinal fusion, the surgeon usually performs two procedures: 1. Implant screws, cages, plates or other stabilizing mechanical constructs to prevent motion between the fused vertebrae 2. Implant bone or bone-inducing products to encourage the patient's natural bone osteoblasts to unite the fused vertebrae, similar to the way a bone fracture heals.
Conditions where spinal fusion may be considered include the following:
- degenerative disc disease
- spinal disc herniation
- discogenic pain
- spinal tumor
- vertebral fracture
- scoliosis
- kyphosis (e. g., Scheuermann's disease)
- spondylolisthesis
- spondylosis
- posterior rami syndrome
- other degenerative spinal conditions
- any condition that causes instability of the spine
Contraindications
Bone morphogenetic protein (rhBMP) should not be routinely used in any type of anterior cervical spine fusion, such as with anterior cervical discectomy and fusion.[2] There are reports of this therapy causing soft tissue swelling, which in turn can cause life-threatening complications due to difficulty swallowing and pressure on the respiratory tract.[2]
Epidemiology
According to a report by the Agency for Healthcare Research and Quality (AHRQ), approximately 488,000 spinal fusions were performed during U.S. hospital stays in 2011 (a rate of 15.7 stays per 10,000 population), which accounted for 3.1% of all operating room procedures.[3] This was a 70 percent growth in procedures from 2001.[4]
Technique
Types of spinal fusion
There are two main types of lumbar spinal fusion, which may be used in conjunction with each other:
Posterolateral fusion places the bone graft between the transverse processes in the back of the spine. These vertebrae are then fixed in place with screws and/or wire through the pedicles of each vertebra attaching to a metal rod on each side of the vertebrae.
Interbody fusion places the bone graft between the vertebra in the area usually occupied by the intervertebral disc. In preparation for the spinal fusion, the disc is removed entirely, for example in ACDF. A device may be placed between the vertebra to maintain spine alignment and disc height. The intervertebral device may be made from either plastic or titanium. The fusion then occurs between the endplates of the vertebrae. Using both types of fusion is known as 360-degree fusion. Fusion rates are higher with interbody fusion. The types of interbody fusion are:
- Anterior lumbar interbody fusion (ALIF)- the disc is accessed from an anterior abdominal incision
- Posterior lumbar interbody fusion (PLIF) – the disc is accessed from a posterior incision
- Transforaminal lumbar interbody fusion (TLIF) – the disc is accessed from a posterior incision on one side of the spine
- Transpsoas interbody fusion (DLIF or XLIF) – the disc is accessed from an incision through the psoas muscle on one side of the spine
- Oblique lateral lumbar interbody fusion (OLLIF) – the disc is accessed from an incision through the psoas muscle obliquely
Procedure
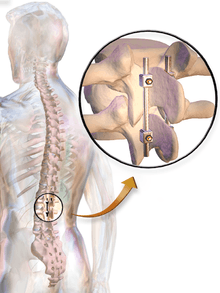
In most cases, the fusion is augmented by a process called fixation, involving the placement of metallic screws (pedicle screws often made from titanium), rods, plates, or cages to stabilize the vertebrae and facilitate bone fusion. The fusion process typically takes 6 to 12 months after surgery. During this time external bracing (orthotics) may be required. External factors such as smoking, osteoporosis, certain medications, and heavy activity can prolong or even prevent the fusion process. If fusion does not occur, patients may require reoperation.
Some newly introduced technologies avoid fusion and preserve spinal motion. Such procedures, such as artificial disc replacement, are alternatives to fusion in the cervical spine. Their advantage over fusion, however, is not well established. Minimally invasive techniques have also been introduced to reduce complications and recovery time for lumbar spinal fusion.[5]
In spinal fusion, the accuracy of screw insertion into the pedicles directly affects surgical outcome. Accurate placement generally involves considerable judgmental skills developed through lengthy training. Because the impact of misaligning one or more pedicle screws can directly affect patient safety, a number of navigational and trajectory verification approaches have been described and evaluated in the literature to provide some degree of guidance to surgeons. For example, Manbachi et. al (2013) presented an overview of the need and the current status of the guidance methods available for improving the surgical outcomes in spinal fusion. They also describe educational aids that have the potential for reducing the training process.[6] Accurate guidance systems, such as the Mazor Robotics "Renaissance", have been developed to assist with spinal fusion procedures.
Society
Frequency of use
According to a report by the Agency for Healthcare Research and Quality (AHRQ), approximately 488,000 spinal fusions were performed during U.S. hospital stays in 2011 (a rate of 15.7 stays per 10,000 population), which accounted for 3.1% of all operating room procedures.[3]
Notable persons who underwent spinal fusion
- Michael Collins, NASA Astronaut
- Phil Jackson, NBA basketball player[7]
- Ryan Kalish, major league baseball player[8]
- Orland Kurtenbach, NHL hockey player[9]
- Peyton Manning, NFL football quarterback[10]
- Lolo Jones, Olympic hurdler[11]
- Jermichael Finley, NFL football tight end[12]
- Andrew "Test" Robert Patrick Martin, Professional Wrestler[13]
- Beth Tweddle, Olympic Medal Winning Gymnast
References
- ↑ "Low Back Disorders (revised 2007)". Occupational Medicine Practice Guidelines (2 ed.). American College of Occupational and Environmental Medicine. 2007. p. 210.
- 1 2 North American Spine Society (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, North American Spine Society, retrieved 25 March 2013, which cites
- Schultz, Daniel G. (July 1, 2008). "Public Health Notifications (Medical Devices) - FDA Public Health Notification: Life-threatening Complications Associated with Recombinant Human Bone Morphogenetic Protein in Cervical Spine Fusion". fda.gov. Retrieved 25 March 2014.
- Woo, EJ (Oct 2012). "Recombinant human bone morphogenetic protein-2: adverse events reported to the Manufacturer and User Facility Device Experience database.". The Spine Journal. 12 (10): 894–9. doi:10.1016/j.spinee.2012.09.052. PMID 23098616.
- 1 2 Weiss AJ, Elixhauser A, Andrews RM (February 2014). "Characteristics of Operating Room Procedures in U.S. Hospitals, 2011.". HCUP Statistical Brief #170. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ Weiss AJ, Elixhauser A (March 2014). "Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011.". HCUP Statistical Brief #171. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ "OLLIF Treatment overview". Retrieved 13 October 2015.
- ↑ Manbachi, A., et al. (2013). Guided pedicle screw insertion: Techniques and training. The Spine Journal 13(4) 1–15.
- ↑ "Phil Jackson". Nba.com. Retrieved November 9, 2013.
- ↑ Mcgair, Brendan. "Red Sox OF Kalish hopes latest surgery does the trick". The Pawtucket Times. Retrieved November 9, 2013.
- ↑ "The NHL's Most Interesting Name: 1960s Part II". Arctic Ice Hockey. Retrieved November 9, 2013.
- ↑ "Spinal fusion surgery: The science behind Manning's life changing operation". News.medill.northwestern.edu. February 2, 2012. Retrieved November 9, 2013.
- ↑ "Cheryl Raye-Stout reviews some key moments from the 2012 Summer Olympic Games in London". Wbez.org. August 13, 2012. Retrieved November 9, 2013.
- ↑ Schwab, Frank (February 6, 2014). "Jermichael Finley excited to play again after spinal fusion surgery | Shutdown Corner". Sports.yahoo.com. Retrieved March 28, 2014.
- ↑ Tweddell, Ross (December 5, 2014). "Andrew 'Test' Martin underwent spinal fusion surgery in July 2004 under Dr. Lloyd Youngblood". Retrieved January 29, 2016 – via whatculture.com.
Further reading
- Cervical Spinal Fusion. WebMD.
- A Patient's Guide to Anterior Cervical Fusion. University of Maryland Medical Center.
- Boatright, K. C. and S. D. Boden. Chapter 12: Biology of Spine Fusion. In: Lieberman, J., et al., Eds. Bone Regeneration and Repair. Totowa, New Jersey: Humana Press. 2005. pp. 225–239. ISBN 978-0-89603-847-9.
- Holmes, C. F., et al. Chapter 9: Cervical Spine Injuries. In: Schenck, R. F., AAOS. Athletic Training in Sports Medicine. Jones & Bartlett Publishers. 2005. pp. 197–218. ISBN 0-89203-172-7
- Camillo, F. X. Chapter 36: Arthrodesis of the Spine. In: Canale, S. T. and J. H. Beaty. Campbell's Operative Orthopaedics 2. (11th Ed.). Philadelphia: Mosby. 2007. pp. 1851–1874. ISBN 978-0-323-03329-9.
- Williams, K. D. and A. L. Park. Chapter 39: Lower Back Pain and Disorders of Intervertebral Discs. In: Canale, S. T. and J. H. Beaty. Campbell's Operative Orthopaedics 2. (11th Ed.). Philadelphia: Mosby. 2007. pp. 2159–2224. ISBN 978-0-323-03329-9.
- Weyreuther, M., et al., Eds. Chapter 7: The Postoperative Spine. MRI Atlas: Orthopedics and Neurosurgery – The Spine. trans. B. Herwig. Berlin: Springer-Verlag. 2006. pp. 273–288. ISBN 978-3-540-33533-7.
- Tehranzadehlow, J., et al. (2005). Advances in spinal fusion. Seminars in Ultrasound, CT, and MRI 26(2): 103–113.
- Resnick, D. K., et al. Surgical Management of Low Back Pain (2nd Ed.). Rolling Meadows, Illinois: American Association of Neurosurgeons. 2008. ISBN 978-1-60406-035-5.
- Oblique Lateral Lumbar Interbody Fusion (OLLIF): Technical Notes and Early Results of a Single Surgeon Comparative Study. NIH.
External links
- Wheeless, C. R., et al., Eds. Fusion of the Spine. Wheeless' Textbook of Orthopaedics. Division of Orthopedic Surgery. Duke University Medical Center.
- Spinal Fusion. American Academy of Orthopaedic Surgeons. June 2010. Accessed 1 June 2013.
- Spinasanta, S. What is Spinal Instrumentation and Spinal Fusion? SpineUniverse. September 2012. Accessed 1 June 2013.
- Spinal fusion. Encyclopedia of Surgery. Accessed 1 June 2013.