Malignant hyperthermia
| Malignant hyperthermia | |
|---|---|
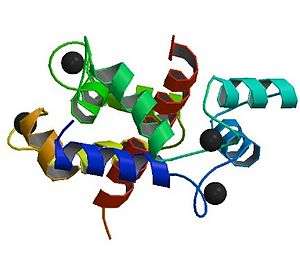 | |
| Abnormalities in the ryanodine receptor 1 gene are commonly detected in people who have experienced an episode of malignant hyperthermia, and may be used to determine the risk of episodes in their relatives | |
| Classification and external resources | |
| Specialty | Anesthesiology, critical care medicine |
| ICD-10 | T88.3 |
| ICD-9-CM | 995.86 |
| OMIM | 145600 154275 154276 600467 601887 601888 |
| DiseasesDB | 7776 |
| MedlinePlus | 001315 |
| MeSH | D008305 |
| GeneReviews | |
Malignant hyperthermia (MH) or malignant hyperpyrexia is a rare life-threatening condition that is usually triggered by exposure to certain drugs used for general anesthesia — specifically the volatile anesthetic agents and succinylcholine, a neuromuscular blocking agent. In susceptible individuals, these drugs can induce a drastic and uncontrolled increase in oxidative metabolism in skeletal muscle, which overwhelms the body's capacity to supply oxygen, remove carbon dioxide, and regulate body temperature, eventually leading to circulatory collapse and death if not immediately treated.
Susceptibility to MH is often inherited as an autosomal dominant disorder, for which there are at least 6 genetic loci of interest,[1] most prominently the ryanodine receptor gene (RYR1). MH susceptibility is phenotypically and genetically related to central core disease (CCD), an autosomal dominant disorder characterized both by MH signs and myopathy. MH is usually revealed upon or shortly after exposure to certain general anesthetic agents. There is no simple, straightforward test to diagnose the condition. Treatment with dantrolene and other drugs is usually initiated when MH is strongly suspected. Dantrolene and the avoidance of triggering agents in susceptible people have markedly reduced the mortality from this condition.
Signs and symptoms
The typical signs of malignant hyperthermia are due to a hypercatabolic state, which presents as a very high temperature, an increased heart rate and abnormally rapid breathing, increased carbon dioxide production, increased oxygen consumption, mixed acidosis, rigid muscles, and rhabdomyolysis.[2] These signs can develop any time during the administration of the anesthetic triggering agents. It is difficult to find confirmed cases in the postoperative period more than several minutes after discontinuation of anesthetic agents.[3]
Causes
Malignant hyperthermia is a disorder that can be considered a gene-environment interaction. In most people with malignant hyperthermia susceptibility, they have few or no symptoms unless they are exposed to a triggering agent. The most common triggering agents are volatile anesthetic gases, such as halothane, sevoflurane, desflurane, isoflurane, enflurane or the depolarizing muscle relaxants suxamethonium and decamethonium used primarily in general anesthesia.[2] In rare cases, the biological stresses of physical exercise or heat may be the trigger.[2][4]
Other anesthetic drugs are considered safe .These include local anesthetics (lidocaine, bupivacaine, mepivacaine), opiates (morphine, fentanyl), ketamine, barbiturates, nitrous oxide, propofol, etomidate, and benzodiazepines.
The nondepolarizing muscle relaxants pancuronium, cisatracurium, atracurium, mivacurium, vecuronium and rocuronium also do not cause MH.
There is mounting evidence that some individuals with malignant hyperthermia susceptibility may develop MH with exercise and/or on exposure to hot environments.[5]
Genetics
Malignant hyperthermia's inheritance is autosomal dominant with variable penetrance.[2] The defect is typically located on the long arm of chromosome 19 (19q13.2[6]) involving the ryanodine receptor.[2] More than 25 different mutations in this gene are linked with malignant hyperthermia.[2] These mutations tend to cluster in one of three domains within the protein, designated MH1-3. MH1 and MH2 are located in the N-terminus of the protein, which interacts with L-type calcium channels and Ca2+
. MH3 is located in the transmembrane forming C-terminus. This region is important for allowing Ca2+
passage through the protein following opening.
Chromosome 7q and chromosome 17 have also been implicated. It has also been postulated that MH and central core disease may be allelic and thus can be co-inherited.
Pathophysiology
Disease mechanism
In a large proportion (50–70%) of cases, the propensity for malignant hyperthermia is due to a mutation of the ryanodine receptor (type 1), located on the sarcoplasmic reticulum (SR), the organelle within skeletal muscle cells that stores calcium.[7][8] RYR1 opens in response to increases in intracellular Ca2+
level mediated by L-type calcium channels, thereby resulting in a drastic increase in intracellular calcium levels and muscle contraction. RYR1 has two sites believed to be important for reacting to changing Ca2+
concentrations: the A-site and the I-site. The A-site is a high affinity Ca2+
binding site that mediates RYR1 opening. The I-site is a lower affinity site that mediates the protein's closing. Caffeine, halothane, and other triggering agents act by drastically increasing the affinity of the A-site for Ca2+
and concomitantly decreasing the affinity of the I-site in mutant proteins. Mg2+
also affect RYR1 activity, causing the protein to close by acting at either the A- or I-sites. In MH mutant proteins, the affinity for Mg2+
at either one of these sites is greatly reduced. The end result of these alterations is greatly increased Ca2+
release due to a lowered activation and heightened deactivation threshold.[9][10] The process of sequestering this excess Ca2+
consumes large amounts of adenosine triphosphate (ATP), the main cellular energy carrier, and generates the excessive heat (hyperthermia) that is the hallmark of the disease. The muscle cell is damaged by the depletion of ATP and possibly the high temperatures, and cellular constituents "leak" into the circulation, including potassium, myoglobin, creatine, phosphate and creatine kinase.
The other known causative gene for MH is CACNA1S, which encodes an L-type voltage-gated calcium channel α-subunit. There are two known mutations in this protein, both affecting the same residue, R1086.[11][12] This residue is located in the large intracellular loop connecting domains 3 and 4, a domain possibly involved in negatively regulating RYR1 activity. When these mutant channels are expressed in human embryonic kidney (HEK 293) cells, the resulting channels are five times more sensitive to activation by caffeine (and presumably halothane) and activate at 5–10mV more hyperpolarized. Furthermore, cells expressing these channels have an increased basal cytosolic Ca2+
concentration. As these channels interact with and activate RYR1, these alterations result in a drastic increase of intracellular Ca2+
, and, thereby, muscle excitability.[13]
Other mutations causing MH have been identified, although in most cases the relevant gene remains to be identified.[1]
Animal model
Research into malignant hyperthermia was limited until the discovery of "porcine stress syndrome" (PSS) in Danish Landrace and other pig breeds selected for muscling, a condition in which stressed pigs develop "pale, soft, exudative" flesh (a manifestation of the effects of malignant hyperthermia) rendering their meat less marketable at slaughter. This "awake triggering" was not observed in humans, and initially cast doubts on the value of the animal model, but subsequently, susceptible humans were discovered to "awake trigger" (develop malignant hyperthermia) in stressful situations. This supported the use of the pig model for research. Pig farmers use halothane cones in swine yards to expose piglets to halothane. Those that die were MH-susceptible, thus saving the farmer the expense of raising a pig whose meat he would not be able to market. This also reduced the use of breeding stock carrying the genes for PSS. The condition in swine is also due to a defect in ryanodine receptors.[14]
Gillard et al. discovered the causative mutation in humans only after similar mutations had first been described in pigs.[7]
Horses also suffer from malignant hyperthermia. A causative mutated allele, ryanodine receptor 1 gene (RyR1) at nucleotide C7360G, generating a R2454G amino acid substitution.[15] has been identified in the American Quarter Horse and breeds with Quarter Horse ancestry, inherited as an autosomal dominant[16][17] It can be caused by overwork, anesthesia, or stress.[18] In dogs, its inheritance is autosomal recessive.[2]
An MH mouse has been constructed, bearing the R163C mutation prevalent in humans. These mice display signs similar to human MH patients, including sensitivity to halothane (increased respiration, body temperature, and death). Blockade of RYR1 by dantrolene prevents adverse reaction to halothane in these mice, as with humans. Muscle from these mice also shows increased K+
-induced depolarization and an increased caffeine sensitivity.[19]
Diagnosis
During an attack
The earliest signs may include: masseter muscle contracture following administration of succinylcholine, a rise in end-tidal carbon dioxide concentration (despite increased minute ventilation), unexplained tachycardia, and muscle rigidity.[2] Despite the name, elevation of body temperature is often a late sign, but may appear early in severe cases. Respiratory acidosis is universally present and many patients have developed metabolic acidosis at the time of diagnosis. A fast rate of breathing (in a spontaneously breathing patient), cyanosis, hypertension, abnormal heart rhythms, and high blood potassium may also be seen. Core body temperatures should be measured in any patient undergoing general anesthesia longer than 30 minutes.
Malignant hyperthermia is diagnosed on clinical grounds, but various laboratory investigations may prove confirmatory. These include a raised creatine kinase level, elevated potassium, increased phosphate (leading to decreased calcium) and—if determined—raised myoglobin; this is the result of damage to muscle cells. Severe rhabdomyolysis may lead to acute kidney failure, so kidney function is generally measured on a frequent basis. Patients may also get premature ventricular contractions due to the increased levels of potassium released from the muscles during episodes.
Susceptibility testing
Muscle testing
The main candidates for testing are those with a close relative who has suffered an episode of MH or has been shown to be susceptible. The standard procedure is the "caffeine-halothane contracture test", CHCT. A muscle biopsy is carried out at an approved research center, under local anesthesia. The fresh biopsy is bathed in solutions containing caffeine or halothane and observed for contraction; under good conditions, the sensitivity is 97% and the specificity 78%.[20] Negative biopsies are not definitive, so any patient who is suspected of MH by their medical history or that of blood relatives is generally treated with nontriggering anesthetics, even if the biopsy was negative. Some researchers advocate the use of the "calcium-induced calcium release" test in addition to the CHCT to make the test more specific.
Less invasive diagnostic techniques have been proposed. Intramuscular injection of halothane 6 vol% has been shown to result in higher than normal increases in local pCO
2 among patients with known malignant hyperthermia susceptibility. The sensitivity was 100% and specificity was 75%. For patients at similar risk to those in this study, this leads to a positive predictive value of 80% and negative predictive value of 100%. This method may provide a suitable alternative to more invasive techniques.[21]
A 2002 study examined another possible metabolic test. In this test, intramuscular injection of caffeine was followed by local measurement of the pCO
2; those with known MH susceptibility had a significantly higher pCO
2 (63 versus 44 mmHg). The authors propose larger studies to assess the test's suitability for determining MH risk.[22]
Genetic testing
Genetic testing is being performed in a limited fashion to determine susceptibility to MH.[2] In people with a family history of MH, analysis for RYR1 mutations may be useful.[1]
Criteria
A 1994 consensus conference led to the formulation of a set of diagnostic criteria. The higher the score (above 6), the more likely a reaction constituted MH:[23]
- Respiratory acidosis (end-tidal CO
2 above 55 mmHg/7.32 kPa or arterial pCO
2 above 60 mmHg/7.98 kPa) - Heart involvement (unexplained sinus tachycardia, ventricular tachycardia or ventricular fibrillation)
- Metabolic acidosis (base excess lower than -8, pH <7.25)
- Muscle rigidity (generalized rigidity including severe masseter muscle rigidity)
- Muscle breakdown (CK >20,000/L units, cola colored urine or excess myoglobin in urine or serum, potassium above 6 mmol/l)
- Temperature increase (rapidly increasing temperature, T >38.8 °C)
- Other (rapid reversal of MH signs with dantrolene, elevated resting serum CK levels)
- Family history (autosomal dominant pattern)
Prevention
In the past, the prophylactic use of dantrolene was recommended for MH susceptible patients undergoing general anesthesia.[24] However, multiple retrospective studies have demonstrated the safety of trigger-free general anesthesia in these patients in the absence of prophylactic dantrolene administration. The largest of these studies looked at the charts of 2214 patients who underwent general or regional anesthesia for an elective muscle biopsy. About half (1082) of the patients were muscle biopsy positive for MH. Only five of these patients exhibited signs consistent with MH, four of which were treated successfully with parenteral dantrolene, and the remaining one recovered with only symptomatic therapy.[25] After weighing its questionable benefits against its possible adverse effects (including nausea, vomiting, muscle weakness and prolonged duration of action of nondepolarising neuromuscular blocking agents[26]), experts no longer recommend the use of prophylactic dantrolene prior to trigger-free general anesthesia in MH susceptible patients.[24]
Anaesthesia for known MH susceptible patients requires avoidance of triggering agents (all volatile anaesthetic agents and succinylcholine). All other drugs are safe (including nitrous oxide), as are regional anaesthetic techniques. Where general anaesthesia is planned, it can be provided safely by removing vaporisers from the anaesthetic machine, placing a new breathing circuit on the machine, flushing the machine and ventilator with 100% oxygen at maximal gas flows for 20–30 minutes, and inducing and maintaining anaesthesia with nontriggering agents (e.g.: propofol).[26] Modern anaesthetic machines have more rubber and plastic components which provide a reservoir for volatile anaesthetics, and should be flushed for 60 minutes.[27]
Charcoal filters can be used to prepare an anesthesia machine for malignant hyperthermia patients in less than 60 seconds. These filters prevent residual anesthetic from triggering malignant hyperthermia for up to 12 hours, even at low fresh gas flows.[28]
Treatment
The current treatment of choice is the intravenous administration of dantrolene, the only known antidote, discontinuation of triggering agents, and supportive therapy directed at correcting hyperthermia, acidosis, and organ dysfunction. Treatment must be instituted rapidly on clinical suspicion of the onset of malignant hyperthermia.[26]
Dantrolene is a muscle relaxant that appears to work directly on the ryanodine receptor to prevent the release of calcium. After the widespread introduction of treatment with dantrolene, the mortality of malignant hyperthermia fell from 80% in the 1960s to less than 5%.[2] Dantrolene remains the only drug known to be effective in the treatment of MH.[24] It is recommended that each hospital keeps a minimum stock of 36 dantrolene vials (720 mg) sufficient for a 70-kg person.[29]
Its clinical use has been limited by its low water solubility, leading to requirements of large fluid volumes, which may complicate clinical management. Azumolene is a 30-fold more water-soluble analogue of dantrolene that also works to decrease the release of intracellular calcium by its action on the ryanodine receptor. In MH susceptible swine, azumolene was as potent as dantrolene.[30] It has yet to be studied in vivo in humans, but may present a suitable alternative to dantrolene in the treatment of MH.

Research in mouse models suggests that azumolene "is likely uncoupling the efficiency of a Ca2+
-dependent RyR1 signal coupled directly or indirectly to the [store-operated calcium entry] machinery." There may be two different pathways of store-operated calcium entry: one, RyR1-reliant and the other, RyR1-non-reliant (see Disease Mechanism section above for RyR1 description). Furthermore, elucidating earlier ideas on the pathogenesis of malignant hyperthermia, researchers point out that it may be "as much a syndrome of exaggerated Ca2+
entry as it is of exaggerated Ca2+
release."[31]
Azumolene has also been shown to be as effective as dantrolene at preventing and reversing contracture in in vitro experiments with human skeletal muscle.[32]
Training
Fast recognition and treatment of MH utilizes skills and procedures that are utilized with a low-frequency and high-risk.[33] Conducting MH crisis training for perioperative teams can identify system failures as well as improve response to these events.[34] Simulation techniques to include the use of cognitive aids have also been shown to improve communication in clinical treatment of MH.[35][36]
Prognosis
Prognosis is poor if this condition is not aggressively treated.[2] In the 1970s, mortality was greater than 80%; with the current management, however, mortality is now less than 5%.[2]
Epidemiology
The incidence is between 1:5,000 to 1:50,000–100,000 procedures involving general anaesthesia.[2] This disorder occurs worldwide and affects all racial groups. Most cases, however, occur in children and young adults, which might be related to the fact many older people will have already had surgeries and thus would know about and be able to avoid this condition.
History
The syndrome was first recognized in Royal Melbourne Hospital, Australia in an affected family by Denborough et al. in 1962.[37][38] Denborough did much of his subsequent work on the condition at the Royal Canberra Hospital.[39] Similar reactions were found in pigs.[40] The efficacy of dantrolene as a treatment was discovered by South African anesthesiologist Gaisford Harrison and reported in a 1975 article published in the British Journal of Anaesthesia.[41] After further animal studies corroborated the possible benefit from dantrolene, a 1982 study confirmed its usefulness in humans.[42]
In 1981, the Malignant Hyperthermia Association of the United States (MHAUS) hotline was established to provide telephone support to clinical teams treating patients with suspected malignant hyperthermia. The hotline became active in 1982 and since that time MHAUS has provided continuous access to board certified anesthesiologists to assist teams in treatment.[43]
Other animals
Other animals, including certain pig breeds, dogs, and horses, are susceptible to malignant hyperthermia.[2]
In dogs its inheritance is autosomal dominant.[44]
In pigs its inheritance is autosomal recessive.[2]
In horses its inheritance is autosomal dominant, and most associated with the American Quarter Horse although it can occur in other breeds.[45]
References
- 1 2 3 Litman R, Rosenberg H; Rosenberg (2005). "Malignant hyperthermia: update on susceptibility testing". JAMA. 293 (23): 2918–24. doi:10.1001/jama.293.23.2918. PMID 15956637.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Rosenberg H, Davis M, James D, Pollock N, Stowell K; Davis; James; Pollock; Stowell (2007). "Malignant hyperthermia". Orphanet J Rare Dis. 2 (1): 21. doi:10.1186/1750-1172-2-21. PMC 1867813
 . PMID 17456235.
. PMID 17456235. - ↑ Litman, Ronald; Flood, Christopher D.; Kaplan, Richard F.; Kim, Yung Ly; Tobin, Joseph R. (November 2008). "Postoperative Malignant Hyperthermia". Anesthesiology. 109 (5): 825–9. doi:10.1097/aln.0b013e31818958e5. PMID 18946294.
- ↑ Groom, Linda; Muldoon, Sheila M.; Tang, Zhen Zhi; Brandom, Barbara W.; Bayarsaikhan, Munkhuu; Bina, Saiid; Lee, Hee-Suk; Qiu, Xing; Sambuughin, Nyamkhishig; Dirksen, Robert T. (November 2011). "Identical de novo Mutation in the Type 1 Ryanodine Receptor Gene Associated with Fatal, Stress-induced Malignant Hyperthermia in Two Unrelated Families". Anesthesiology. 115 (5): 938–45. doi:10.1097/aln.0b013e3182320068. PMID 21918424.
- ↑ H Rosenberg, N Sambuughin, S Riazi, R Dirksen; Sambuughin; Riazi; Dirksen; Pagon; Adam; Ardinger; Wallace; Amemiya; Bean; Bird; Dolan; Fong; Smith; Stephens (2013). "Malignant Hyperthermia Susceptibility". GeneReviews. PMID 20301325.
- ↑ "OMIM Entry - * 180901 - RYANODINE RECEPTOR 1; RYR1". www.omim.org. Retrieved 2016-01-06.
- 1 2 Gillard E, Otsu K, Fujii J, Khanna V, de Leon S, Derdemezi J, Britt B, Duff C, Worton R, MacLennan D; Otsu; Fujii; Khanna; De Leon; Derdemezi; Britt; Duff; Worton; MacLennan (1991). "A substitution of cysteine for arginine 614 in the ryanodine receptor is potentially causative of human malignant hyperthermia". Genomics. 11 (3): 751–5. doi:10.1016/0888-7543(91)90084-R. PMID 1774074.
- ↑ Galli L, Orrico A, Lorenzini S, Censini S, Falciani M, Covacci A, Tegazzin V, Sorrentino V; Orrico; Lorenzini; Censini; Falciani; Covacci; Tegazzin; Sorrentino (2006). "Frequency and localization of mutations in the 106 exons of the RYR1 gene in 50 individuals with malignant hyperthermia". Hum Mutat. 27 (8): 830. doi:10.1002/humu.9442. PMID 16835904.
- ↑ Balog E, Fruen B, Shomer N, Louis C; Fruen; Shomer; Louis (2001). "Divergent effects of the malignant hyperthermia-susceptible Arg(615)-->Cys mutation on the Ca(2+) and Mg(2+) dependence of the RyR1". Biophys J. 81 (4): 2050–8. Bibcode:2001BpJ....81.2050B. doi:10.1016/S0006-3495(01)75854-7. PMC 1301678
 . PMID 11566777.
. PMID 11566777. - ↑ Yang T, Ta T, Pessah I, Allen P; Ta; Pessah; Allen (2003). "Functional defects in six ryanodine receptor isoform-1 (RyR1) mutations associated with malignant hyperthermia and their impact on skeletal excitation-contraction coupling". J Biol Chem. 278 (28): 25722–30. doi:10.1074/jbc.M302165200. PMID 12732639.
- ↑ Monnier N, Procaccio V, Stieglitz P, Lunardi J; Procaccio; Stieglitz; Lunardi (1997). "Malignant-hyperthermia susceptibility is associated with a mutation of the alpha 1-subunit of the human dihydropyridine-sensitive L-type voltage-dependent calcium-channel receptor in skeletal muscle". Am J Hum Genet. 60 (6): 1316–25. doi:10.1086/515454. PMC 1716149
 . PMID 9199552.
. PMID 9199552. - ↑ The R1086C mutant has never been published, but has nevertheless been referenced multiple times in the literature, e.g. Jurkat-Rott K, McCarthy T, Lehmann-Horn F; McCarthy; Lehmann-Horn (2000). "Genetics and pathogenesis of malignant hyperthermia". Muscle Nerve. 23 (1): 4–17. doi:10.1002/(SICI)1097-4598(200001)23:1<4::AID-MUS3>3.0.CO;2-D. PMID 10590402.
- ↑ Weiss R, O'Connell K, Flucher B, Allen P, Grabner M, Dirksen R; O'Connell; Flucher; Allen; Grabner; Dirksen (2004). "Functional analysis of the R1086H malignant hyperthermia mutation in the DHPR reveals an unexpected influence of the III-IV loop on skeletal muscle EC coupling". Am J Physiol Cell Physiol. 287 (4): C1094–102. doi:10.1152/ajpcell.00173.2004. PMID 15201141.
- ↑ J Fujii; K Otsu; F Zorzato; S de Leon; VK Khanna; JE Weiler; PJ O'Brien; DH MacLennan (1991). "Identification of a mutation in porcine ryanodine receptor associated with malignant hyperthermia". Science. 253 (5018): 448–451. Bibcode:1991Sci...253..448F. doi:10.1126/science.1862346. PMID 1862346.
- ↑ Aleman M, Nieto JE, Magdesian KG; Nieto; Magdesian (2009). "Malignant hyperthermia associated with ryanodine receptor 1 (C7360G) mutation in Quarter Horses". J. Vet. Intern. Med. 23 (2): 329–34. doi:10.1111/j.1939-1676.2009.0274.x. PMID 19220734.
- ↑ http://manc.umd.edu/Abstracts2010/LenzHYPP%20abstract.pdf
- ↑ ftp://ftp.aave.inv.org.ar/IVIS/aaep/Equine%20Malignant%20Hyperthermia.pdf
- ↑ Valberg SJ, Mickelson JR, Gallant EM, MacLeay JM, Lentz L, de la Corte F; Mickelson; Gallant; MacLeay; Lentz; de la Corte (1999). "Exertional rhabdomyolysis in quarter horses and thoroughbreds: one syndrome, multiple aetiologies". Equine Vet J Suppl. 30 (30): 533–8. PMID 10659313.
- ↑ Yang T, Riehl J, Esteve E, et al. (2006). "Pharmacologic and functional characterization of malignant hyperthermia in the R163C RyR1 knock-in mouse". Anesthesiology. 105 (6): 1164–75. doi:10.1097/00000542-200612000-00016. PMID 17122579.
- ↑ Allen G, Larach M, Kunselman A; Larach; Kunselman (1998). "The sensitivity and specificity of the caffeine-halothane contracture test: a report from the North American Malignant Hyperthermia Registry". Anesthesiology. 88 (3): 579–88. doi:10.1097/00000542-199803000-00006. PMID 9523799.
- ↑ Schuster F, Gardill A, Metterlein T, Kranke P, Roewer N, Anetseder M; Gardill; Metterlein; Kranke; Roewer; Anetseder (2007). "A minimally invasive metabolic test with intramuscular injection of halothane 5 and 6 vol% to detect probands at risk for malignant hyperthermia". Anaesthesia. 62 (9): 882–7. doi:10.1111/j.1365-2044.2007.05173.x. PMID 17697213.
- ↑ Anetseder M, Hager M, Müller CR, Roewer N; Hager; Müller; Roewer (2002). "Diagnosis of susceptibility to malignant hyperthermia by use of a metabolic test". Lancet. 359 (9317): 1579–80. doi:10.1016/S0140-6736(02)08506-9. PMID 12047971.
- ↑ Larach MG, Localio AR, Allen GC, et al. (1994). "A clinical grading scale to predict malignant hyperthermia susceptibility". Anesthesiology. 80 (4): 771–9. doi:10.1097/00000542-199404000-00008. PMID 8024130.
- 1 2 3 Krause T, Gerbershagen MU, Fiege M, Weisshorn R, Wappler F; Gerbershagen; Fiege; Weisshorn; Wappler (2004). "Dantrolene--a review of its pharmacology, therapeutic use and new developments". Anaesthesia. 59 (4): 364–73. doi:10.1111/j.1365-2044.2004.03658.x. PMID 15023108.
- ↑ Carr AS, Lerman J, Cunliffe M, McLeod ME, Britt BA; Lerman; Cunliffe; McLeod; Britt (1995). "Incidence of malignant hyperthermia reactions in 2,214 patients undergoing muscle biopsy". Can J Anaesth. 42 (4): 281–6. doi:10.1007/BF03010703. PMID 7788824.
- 1 2 3 Halsall PJ, Hopkins PM; Hopkins (2003). "Malignant hyperthermia". Continuing Education in Anaethesia, Critical Care and Pain. 3 (1): 5–9. doi:10.1093/bjacepd/mkg002.
- ↑ Kim Tae W., Nemergut, ME; Nemergut (2011). "Preparation of Modern Anesthesia Workstations for Malignant Hyperthermia–susceptible Patients: A Review of Past and Present Practice". Anesthesiology. 114 (1): 205–212. doi:10.1097/ALN.0b013e3181ee2cb7. PMID 21169802.
- ↑ Stoker, Robert; Romankowski, Mathew; Burk, Kyle; Orr, Joseph (October 15, 2013). "12 Hour Evaluation of Filters to Prepare an Anesthesia Machine for Malignant Hyperthermia Susceptible Patients" (Abstract# A4094). Anesthesiology 2013 Annual Meeting.
- ↑ EYH Yeung, Munroe J; Munroe (2015). "Development of a malignant hyperthermia protocol" (PDF). BMC Proceedings. 9 (Suppl1): A32. doi:10.1186/1753-6561-9-S1-A32 (inactive 2015-06-09). PMC 4306034
 .
. - ↑ Dershwitz M, Sréter FA; Sréter (1990). "Azumolene reverses episodes of malignant hyperthermia in susceptible swine". Anesth. Analg. 70 (3): 253–5. doi:10.1213/00000539-199003000-00004. PMID 2305975.
- ↑ Zhao X, Weisleder N, Han X, Pan Z, Parness J, Brotto M, Ma J; Weisleder; Han; Pan; Parness; Brotto; Ma (2006). "Azumolene Inhibits a Component of Store-operated Calcium Entry Coupled to the Skeletal Muscle Ryanodine Receptor". The Journal of Biological Chemistry. 281 (44): 33477–86. doi:10.1074/jbc.M602306200. PMID 16945924.
- ↑ Sudo RT, Carmo, PL, Trachez MM, Pan Z, Zapata-Sudo G; Carmo; Trachez; Zapata-Sudo (2008). "Effects of Azumolene on Normal and Malignant Hyperthermia-Susceptible Skeletal Muscle". Basic & Clinical Pharmacology & Toxicology. 102 (3): 308–16. doi:10.1111/j.1742-7843.2007.00156.x. PMID 18047479.
- ↑ Cain CL, Riess ML, Gettrust L, Novalija J (2014). "Malignant hyperthermia crisis: optimizing patient outcomes through simulation and interdisciplinary collaboration". AORN Journal. 99 (2): 301–8; quiz 309–11. doi:10.1016/j.aorn.2013.06.012. PMC 4276305
 . PMID 24472592. Retrieved 2015-12-24.
. PMID 24472592. Retrieved 2015-12-24. - ↑ Hirshey Dirksen SJ, Van Wicklin SA, Mashman DL, Neiderer P, Merritt DR (2013). "Developing effective drills in preparation for a malignant hyperthermia crisis". AORN Journal. 97 (3): 329–53. doi:10.1016/j.aorn.2012.12.009. PMID 23452698. Retrieved 2015-12-24.
- ↑ Isaak RS, Stiegler MP (2015). "Review of crisis resource management (CRM) principles in the setting of intraoperative malignant hyperthermia". Journal of Anesthesia. doi:10.1007/s00540-015-2115-8. PMID 26679497. Retrieved 2015-12-28.
- ↑ Holzman RS, Cooper JB, Gaba DM, Philip JH, Small SD, Feinstein D (1995). "Anesthesia crisis resource management: real-life simulation training in operating room crises". Journal of Clinical Anesthesia. 7 (8): 675–87. doi:10.1016/0952-8180(95)00146-8. PMID 8747567. Retrieved 2015-12-24.
- ↑ http://www.anaesthesia.mh.org.au/mh-discovered-at-rmh/w1/i1002827/
- ↑ Denborough MA, Forster JF, Lovell RR, Maplestone PA, Villiers JD; Forster; Lovell; Maplestone; Villiers (1962). "Anaesthetic deaths in a family". British Journal of Anaesthesia. 34 (6): 395–6. doi:10.1093/bja/34.6.395. PMID 13885389. Historical account in Denborough MA (2008). "Malignant hyperthermia. 1962". Anesthesiology. 108 (1): 156–7. doi:10.1097/01.anes.0000296107.23210.dd. PMID 18156894.
- ↑ Malcolm Whyte. 'Clinical Science in Canberra Hospital' in AJ Proust (ed) History of Medicine in Canberra and Queanbeyan and their Hospitals Brolga Press, Gundaroo p123 at 127
- ↑ Hall LW, Woolf N, Bradley JW, Jolly DW; Woolf; Bradley; Jolly (1966). "Unusual reaction to suxamethonium chloride". Br Med J. 2 (5525): 1305. doi:10.1136/bmj.2.5525.1305. PMC 1944316
 . PMID 5924819.
. PMID 5924819. - ↑ Harrison GG (January 1975). "Control of the malignant hyperpyrexic syndrome in MHS swine by dantrolene sodium". British Journal of Anaesthesia. 47 (1): 62–5. doi:10.1093/bja/47.1.62. PMID 1148076. A reprint of the article, which became a "Citation Classic", is available in Br J Anaesth81 (4): 626–9. PMID 9924249 (free full text).
- ↑ Kolb ME, Horne ML, Martz R; Horne; Martz (1982). "Dantrolene in human malignant hyperthermia". Anesthesiology. 56 (4): 254–62. doi:10.1097/00000542-198204000-00005. PMID 7039419.
- ↑ Dexter F, Rosenberg H, Epstein RH, Semo JJ, Litman RS (2015). "Implications of National Anesthesia Workload on the Staffing of a Call Center: The Malignant Hyperthermia Consultant Hotline". A&A Case Reports. 5 (3): 43–6. doi:10.1213/XAA.0000000000000147. PMID 26230307. Retrieved 2015-12-24.
- ↑ Roberts, M. C.; Mickelson, J. R.; Patterson, E. E.; Nelson, T. E.; Armstrong, P. J.; Brunson, D. B.; Hogan, K (Sep 2001). "Autosomal dominant canine malignant hyperthermia is caused by a mutation in the gene encoding the skeletal muscle calcium release channel (RYR1)". Anesthesiology. 95 (3): 716–25. doi:10.1097/00000542-200109000-00026. PMID 11575546.
- ↑ Mickelson JR, Valberg SJ. (2015). "The Genetics of Skeletal Muscle Disorders in Horses". Annu. Rev. Anim. Biosci. 3: 197–217.
External links
- GeneReview/NIH/UW entry on Malignant Hyperthermia Susceptibility
- Malignant Hyperthermia Association of the United States
- Making Anesthesia Safer - Unraveling the Malignant Hyperthermia Puzzle by Marilyn Green Larach, FASEB "Breakthroughs in Bioscience"