Oculocerebrorenal syndrome
| Oculocerebrorenal syndrome | |
|---|---|
| Classification and external resources | |
| ICD-10 | E72.0 |
| ICD-9-CM | 270.8 |
| OMIM | 309000 |
| DiseasesDB | 29146 |
| eMedicine | oph/516 |
| MeSH | D009800 |
| GeneReviews | |
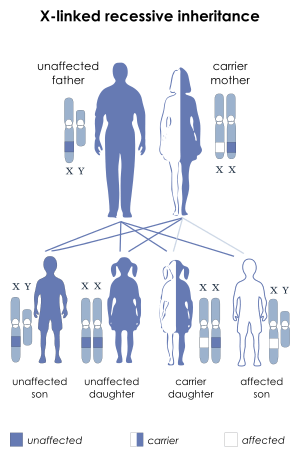
Oculocerebrorenal syndrome (also called Lowe syndrome) is a rare X-linked recessive disorder characterized by congenital cataracts, hypotonia and areflexia, intellectual disability, proximal tubular acidosis, aminoaciduria, phosphaturia, and low-molecular-weight proteinuria. Glaucoma is present in about 50% of cases.
Lowe syndrome can be considered a cause of Fanconi syndrome (bicarbonaturia, renal tubular acidosis, aminoaciduria, phosphaturia, tubular proteinuria, and impaired urine-concentrating ability).[1]
Presentation
Because it is an X-linked recessive condition, the disease develops mostly in men with very rare occurrences in women, while women are carriers of the disease. It has an estimated prevalence of 1 in 500,000 people.[2] Boys with Lowe syndrome are born with cataracts in both eyes (the hallmark of the disease). Glaucoma is present in about 50% of the patients with Lowe syndrome, though usually not at birth. While not present at birth, many affected boys develop kidney problems at about one year of age. Renal pathology is characterized by an abnormal loss of certain substances into the urine, including bicarbonate, sodium, potassium, amino acids, organic acids, albumin and other small proteins, calcium, phosphate, glucose, and L-carnitine. This problem, known as Fanconi-type renal tubular dysfunction, can also be seen in other diseases and syndromes.
Genetics
This syndrome is caused by mutations in the OCRL1 gene which encodes a inositol polyphosphate-5-phosphatase.[3] At least one mechanism by which these mutations cause this syndrome is by loss of its Rab binding domain.[4] This protein is associated with the primary cilia of the retinal pigment epithelial cells, fibroblasts and kidney tubular cells.[5] This suggests that this syndrome is due to dysfunction of the cilia in these cells.[6]
History
It was first described in 1952 by Charles Lowe and colleagues at the Massachusetts General Hospital in Boston.[7] Because of the three major organ systems involved (eyes, brain, and kidney), it is also known as oculocerebrorenal syndrome.
Eponym
It is named after Charles Upton Lowe (August 24, 1921 – February 9, 2012 ).[8]
References
- ↑ Vilasi A, Cutillas PR, Maher AD, et al. (August 2007). "Combined proteomic and metabonomic studies in three genetic forms of the renal Fanconi syndrome". Am. J. Physiol. Renal Physiol. 293 (2): F456–67. doi:10.1152/ajprenal.00095.2007. PMID 17494094.
- ↑ Loi M. Lowe Syndrome. Orphanet Journal of Rare Diseases 2006,1:16
- ↑ Kanık A, Kasap-Demir B, Ateşli R, Eliaçık K, Yavaşcan O, Helvacı M (2013) A novel OCRL1 gene mutation in a Turkish child with Lowe syndrome. The Turkish Journal of Pediatrics 55(1):82-85
- ↑ Hagemann N, Hou X, Goody RS, Itzen A, Erdmann KS (2012) Crystal structure of the Rab binding domain of OCRL1 in complex with Rab8 and functional implications of the OCRL1/Rab8 module for Lowe syndrome. Small GTPases 3(2):107-10. doi: 10.4161/sgtp.19380
- ↑ Luo N, West CC, Murga-Zamalloa CA, Sun L, Anderson RM, Wells CD, Weinreb RN, Travers JB, Khanna H, Sun Y (2012) OCRL localizes to the primary cilium: a new role for cilia in Lowe syndrome. Hum Mol Genet 21(15):3333-3344 doi: 10.1093/hmg/dds163
- ↑ Rbaibi Y, Cui S, Mo D, Carattino M, Rohatgi R, Satlin LM, Szalinski CM, Swanhart LM, Fölsch H, Hukriede NA, Weisz OA. OCRL1 modulates cilia length in renal epithelial cells. Traffic 13(9):1295-305. doi: 10.1111/j.1600-0854.2012.01387.x
- ↑ Lowe CU, Terrey M, MacLachlan EA (1952). "Organic-aciduria, decreased renal ammonia production, hydrophthalmos, and mental retardation; a clinical entity". AMA American Journal of Diseases of Children. 83 (2): 164–84. PMID 14884753.
- ↑ synd/3512 at Who Named It?
External links
- Lowe Syndrome Association official website
- U.K. Lowe Syndrome Trust
- GeneReview/NIH/UW entry on Lowe syndrome