Cryoneurolysis
Cryoneurolysis, also referred to as cryoanalgesia, cryoneuromodulation, or cryoneuroablation, is a procedure used to temporarily block nerve conduction along peripheral nerve pathways. The procedure, which involves insertion of a small probe to freeze the target nerve, allows for the complete regeneration of the structure and function of the affected nerve. Cryoneurolysis has been used to treat a variety of painful conditions including.
Medical uses
A similar procedure using radiofrequency for back pain appears to have short term benefit but it is unclear if it has any long term effect.[1]
Mechanisms of action
Nerve anatomy
Each nerve is composed of a bundle of axons. Each axon is surrounded by the endoneurium connective tissue layer. These axons are bundled into fascicles which are surrounded by the perineurium connective tissue layer. Multiple fascicles are then surrounded by the epineurium, which is the outermost connective tissue layer of the nerve. The axons of myelinated nerves have a myelin sheath made up of Schwann cells that coat the axon.[2]
Nerve injury classification
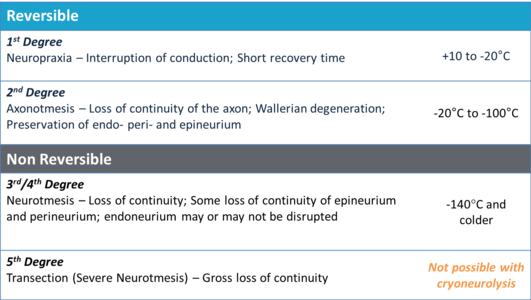
The classifications of nerve damage have been well-defined by Sir Herbert Seddon and Sunderland and are still in use today.[6] The table at the right details the forms (neurapraxia, axonotmesis and neurotmesis) and degrees of nerve injury that occur as a result of exposure to various temperatures.
Cryoneurolysis treatments which utilize nitrous oxide (boiling point of -88.5 °C) as the coolant fall in the range of an axonotmesis injury, or 2nd degree injury according to the Sunderland classification system. Treatments of the nerve in this temperature range are reversible. Nerves treated in this temperature range experience a disruption of the axon, with Wallerian degeneration occurring distal to the site of injury.[7] The axon and myelin sheath are affected, but all of the connective tissues (endoneurium, perineurium, and epineurium) remain intact.[8] Following Wallerian degeneration the axon regenerates along the original nerve path at a rate of approximately 1–2 mm per day.[9][10][11][12]
Cryoneurolysis treatments which utilize liquid nitrogen (boiling point of -195.8 °C) as the coolant fall into the range of a neurotmesis injury, or 3rd degree injury according to the Sunderland classification. Treatments of the nerve in this temperature range are irreversible. Nerves treated in this temperature range experience a disruption of both the axon and the endoneurium connective tissue layer.[13][14]
History
The use of cold for pain relief and as an anti-inflammatory has been known since the time of Hippocrates (460-377 B.C).[15] Since then there have been numerous accounts of ice used for pain relief including from the Ancient Egyptians and Avicenna of Persia (A.D.982–1070).[16] In 1812 Napoleon's Surgeon General noted that half-frozen soldiers from the Moscow battle were able to tolerate amputations with reduced pain[17] and in 1851, ice and salt mixtures were promoted by Arnott for the treatment of nerve pain. Campbell White, in 1899, was the first to employ refrigerants for medical use and Allington, in 1950, was the first to use liquid nitrogen for medical treatments.[15] In 1961, Cooper et al. created an early cryoprobe, which reached a temperature of -190 °C using liquid nitrogen.[15] Shortly thereafter, in 1967, an ophthalmic surgeon named Amoils used carbon dioxide and nitrous oxide to create a cryoprobe which reached a temperature of -70 °C.[15]
Devices
Cryoprobe
Cryoneurolysis is performed with a cryoprobe, which is composed of a hollow cannula that contains a smaller inner lumen. The pressurized coolant (nitrous oxide or liquid nitrogen) travels down the lumen and expands at the end of the lumen into the tip of the hollow cannula. No coolant exits the cryoprobe. The expansion of the pressurized liquid causes the surrounding area to cool (known as the Joule-Thomson effect) and the phase change of the liquid to gas also causes the surrounding area to cool. This causes a visible iceball to form and the tissue surrounding the end of the cryoprobe to freeze. The gas form of the coolant then travels up the length of the cryoprobe and is safely expelled. The tissue surrounding the end of the cryoprobe can reach a temperature as low as -88.5 °C when nitrous oxide is used as the coolant and can reach a temperature as low as -195.8 °C when liquid nitrogen is used as the coolant.
Devices
The Endocare PerCryo Percutaneous Cryoablation device utilizes argon as a coolant and can be used with 4 different single cryoprobe configurations with a diameter of either 1.7 mm (~16 gauge) or 2.4 mm (~13 gauge) in diameter .[18]
The Myoscience Iovera° is a handheld device that uses nitrous oxide as a coolant and can be used with a three-probe configuration with a probe diameter of 0.4 mm (~27 gauge).[19]
References
- ↑ Boswell, MV; Colson, JD; Sehgal, N; Dunbar, EE; Epter, R (January 2007). "A systematic review of therapeutic facet joint interventions in chronic spinal pain.". Pain physician. 10 (1): 229–53. PMID 17256032.
- ↑ Gray, Henry (1918). Gray's Anatomy. Philadelphia: Lea & Febiger. ISBN 1-58734-102-6.
- ↑ Zhou (1995). "Mechanism research of cryoanalgesia". Neurological Research. 17 (4): 301–311. PMID 7477749.
- ↑ Sunderland (1968). Nerves and Nerve Injuries. Edinburgh & London: Livingstone. p. 180.
- ↑ Zhou (2003). "Cryoanalgesia: electrophysiology at different temperatures". Cryobiology. 46: 26–32. doi:10.1016/s0011-2240(02)00160-8.
- ↑ Seddon HJ (1943). "Three Types of Nerve Injury". Brain. 66 (4): 238–288. doi:10.1093/brain/66.4.237.
- ↑ Savastano (2014). "Sciatic nerve injury: A simple and subtle model for investigating many aspects of nervous system damage and recovery". Journal of Neuroscience Methods. 227: 166–180. doi:10.1016/j.jneumeth.2014.01.020.
- ↑ Hsu (2013). "Reduction in muscular motility by selective focused cold therapy". Journal of Neural Transmission. 121 (1): 15–20. doi:10.1007/s00702-013-1077-y. PMID 23917804.
- ↑ Evans (1981). "Cryoanalgesia: the response to alterations in freeze cycle and temperature". British Journal of Anesthesiology. 53 (11): 1121–1127. doi:10.1093/bja/53.11.1121.
- ↑ Tetzlaff (1989). "Neurofilament elongation into regenerating facial nerve axons". Neuroscience. 29 (3): 659–666. doi:10.1016/0306-4522(89)90138-3.
- ↑ Seil (1983). Nerve, organ, and tissue regeneration--research perspectives (xv ed.). New York: Academic Press. p. 482.
- ↑ Lundy-Eckman (2007). Neuroscience: Fundamentals for rehabilitation (3rd ed.). St. Louis, MIssouri: Elsevier Saunders.
- ↑ Sunderland (1951). "A classification of peripheral nerve injuries producing loss of function". Brain. 74 (4): 491–516. doi:10.1093/brain/74.4.491.
- ↑ Burnett (2004). "Pathophysiology of peripheral nerve injury: a brief review". Neurosurgical Focus. 16 (5): E1. doi:10.3171/foc.2004.16.5.2.
- 1 2 3 4 Cooper (2001). "The History of Cryosurgery". J R Soc Med. 94 (4): 196–201.
- ↑ Trescott (2003). "Cryoanalgesia in Interventional Pain Management". Pain Physician. 6: 345–360.
- ↑ Larrey, Dominique Jean (1832). Surgical Memoirs of the campaigns of Russia, Germany and France. Philadelphia: Carey & Lea.
- ↑ "The perfect Percryo probe for any procedure" (PDF). http://www.healthtronics.com. Retrieved April 11, 2015. External link in
|website=(help) - ↑ "Iovera Health - How it Works". http://www.myoscience.com. Retrieved April 11, 2015. External link in
|website=(help)